
As a payer, provider, pharma or government healthcare services provider, you have unique and evolving customer management needs. And thanks to companies like Netflix, Amazon and Uber, your patients expect a more seamless digital experience.
That means you need to excel not only across traditional engagement channels but across digital channels as well—while still offering a human touch when patients are at their most vulnerable.
At Faneuil, we create patient-centric solutions that meet those needs and comply with all legal and industry guidelines. This seamless healthcare experience digitally integrates with the lifestyles of your members and patients and provides support when they’re facing difficult circumstances.
Our highly skilled advocates undergo extensive training in the classroom and in closely supervised, on-the-job settings to help them provide compassionate, accurate, complete and timely care.
We ensure they understand the importance of their role in the healthcare industry and are passionate about the people and communities they serve.
Health Plans — Provider and Pharmaceutical
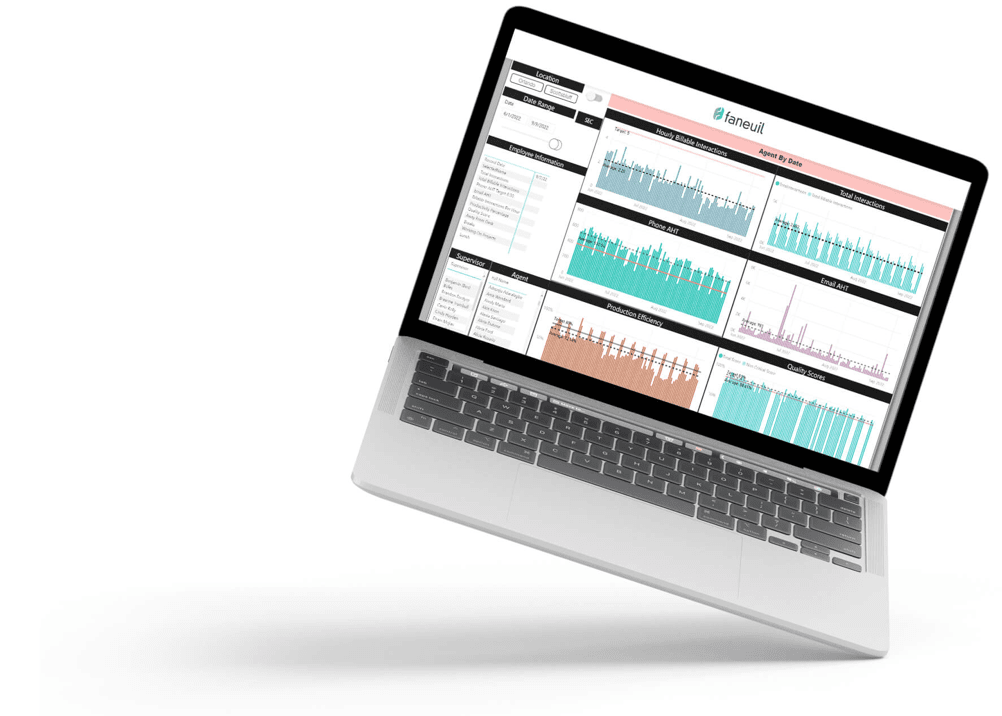
To provide human-centric support, our advocates are empowered with best-in-class technology and a digital innovation suite that includes artificial intelligence and powerful analytics capabilities.
HEALTH PLANS
Member and Provider Services
We cover all lines of business, including Medicare, Medicaid and individual and family plans. Our expertise spans from critical first impressions formed during enrollment through member services, proactive health management and retention. We also support providers by answering questions about eligibility, copays and claim status.
Complex problems are solved accurately and with empathy throughout the healthcare journey. And our advocates harness the power of technology to ensure every interaction is as efficient, consistent and personal as your members and providers expect.
SALES
Healthcare can be complicated and confusing. It requires a skilled agent to explain complex products in an easy-to-understand way. Additionally, sales agents need specific certifications and skills, which vary by plan type and state. And staffing is a challenge because it’s difficult to accurately predict call demand.
We have the experience to support health plans with their licensed sales agent requirements.
IN-HOME
Build strong connections with your members by reaching people where traditional healthcare does not: in their homes and communities.
Our work makes healthcare more accessible and convenient and allows critical care and social gaps to be closed. This enables you to provide a better member experience while improving quality, cost and outcomes.
PHARMACEUTICAL
Our member-focused service model quickly connects members to a live person committed to first-call resolution.
We help your members manage their medication requirements and pharmacy benefits. Whether simply seeking a refill, checking a mail order status or handling more complex needs related to out-of-medication or alternative medication situations, our experts are on-hand to proactively support your members and be the bridge between the provider, pharmacy and health plan.
